I. Introduction
The burgeoning field of digital pathology has created a surge, a maelstrom, a hurricane if you will of publications detailing its implementation within pathology workflows. However, a discernible gap
The burgeoning field of digital pathology has created a surge, a maelstrom, a hurricane if you will of publications detailing its implementation within pathology workflows. However, a discernible gap
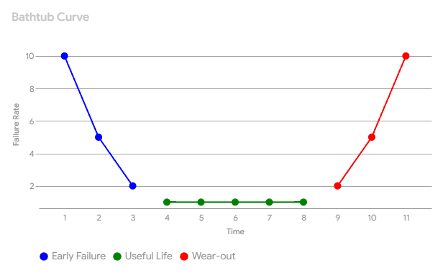
exists between the theoretical advocacy for digital pathology and its pragmatic application in clinical diagnostic settings. This article, informed by experience in implementing digital pathology systems in diagnostic environments, aims to bridge this gap by examining the implementation process through the lens of the "bathtub curve" – a concept borrowed from reliability engineering that depicts the failure rate of a product or system over its lifespan. By applying this framework, we offer insights into establishing and maintaining working pathology systems that effectively meet the evolving demands of the laboratory and contribute to enhanced patient care.
For Reliability Engineering purposes, the curve is divided into three distinct phases:
Similar to most technological implementations, the journey towards a digital pathology lab is not without its challenges. These challenges often follow the same predictable pattern. The bathtub curve provides a valuable framework for understanding the phases of digital pathology implementation. Here's how it connects:
II. The "Left Side" of the Tub: Early Implementation Challenges
In the beginning phases of digital pathology implementation, users will typically encounter a series of technical and workflow-related obstacles. Technical considerations primarily revolve around image quality and scanner variability. While certain scanners demonstrate superior performance in capturing specific features, such as H. pylori organisms, others may exhibit limitations when digitizing cytology specimens. Even with FDA-approved, high-end scanners, suboptimal images can occur, manifesting as blur, artifacts, or inconsistencies due to factors such as poor coverslipping, tissue folds, or debris on the slide.
Implementing a robust and user-friendly scanner calibration system is essential for achieving consistent and reliable image quality. Automated calibration enables control over color rendering, staining intensity representation, and tissue visualization. By promptly identifying and correcting performance deviations, such a system ensures the acquisition of high-quality images suitable for rigorous analysis and interpretation. This enhances the accuracy and reliability of image-based data in research and clinical settings.
While artificial intelligence (AI) solutions offer promising tools for quality control in digital pathology, their performance is not yet flawless. It is important to acknowledge that many current systems employ augmented intelligence approaches, often lacking true neural network architecture. These systems rely on predefined rules and algorithms to identify potential quality issues, which can lead to limitations in their adaptability and accuracy, especially when faced with the complexity and variability of histological preparations.
Consequently, augmented intelligence systems in digital pathology often require human oversight and intervention. Technicians may need to review and validate the quality assessments made by the system, potentially leading to rescans or image adjustments. Despite these limitations, augmented intelligence tools can still significantly benefit digital pathology workflows by automating initial quality checks and assisting technicians in identifying areas that require further attention. As AI technology continues to evolve, we can expect integrated explainability, with more robust and adaptable solutions that further enhance quality control processes in digital pathology.
To fully harness the transformative potential of AI in digital pathology, a forward-thinking approach to implementation is essential. Pathologists should proactively engage in strategic planning that encompasses current and future AI requirements, recognizing the evolving nature of AI algorithms and their expanding applications within the field. This provides a thorough evaluation of scanner compatibility with a spectrum of algorithms, ensuring the chosen system possesses the capacity for integration with both existing and emerging image tools. Moreover, the computational burden imposed by AI mandates consideration of data storage and processing infrastructure. A failure to adequately provision for these demands can bring performance bottlenecks and impede the realization of AI's full capabilities within the pathology workflow.
The integration of digital pathology with existing laboratory information systems (LIS), electronic health records (EHR), and hospital information systems (HIS) presents significant challenges. Maintaining data integrity is paramount, and rigorous validation is necessary to ensure the accurate transfer of information between these systems. Of particular concern is the potential for discrepancies between scanned microscopic areas and their corresponding macroscopic images. Such errors, which I have observed firsthand, underscore the current limitations within the field of digital pathology and highlight the critical need for high-quality manufacturing processes, stringent data integrity validation, and continuous system monitoring.
Furthermore, limitations in network bandwidth and storage capacity can impede seamless workflow. Inadequate planning for rescans and duplicate images can overwhelm local storage solutions (e.g., servers, USB backups, network-attached storage), while inefficient data management practices can lead to increased cloud storage costs. Software bugs and compatibility issues can also arise, requiring proactive troubleshooting and vendor support.
Proactively addressing potential challenges and implementing robust workflows are crucial for smooth transitions. A common hurdle, as many of us have experienced, is staff resistance to new technology. I recall a specific instance a few years ago involving a senior neuropathologist who initially favored traditional microscopy for visualizing subtle neuronal inclusions, believing digital pathology lacked the necessary detail. This presented an opportunity to emphasize the importance of comprehensive training, and with appropriate workflow adjustments, the neuropathologist quickly became a proponent of digital pathology. Such transitions often require ongoing support and patience. Fortunately, continuous advancements in scanner technology, staining techniques, and AI-powered image analysis are steadily enhancing the visualization and analysis of even the most subtle microscopic features.
Successful implementation of digital pathology extends beyond technical considerations and necessitates the establishment of standardized protocols and robust security measures to address concerns around data privacy and cybersecurity. Within healthcare, collaboration with a vendor who prioritizes patient information protection and possesses a thorough understanding of cybersecurity threats is crucial. This includes demonstrated compliance and understanding of relevant regulations like HIPAA, use of robust security measures such as encryption and access controls, transparency and accountability regarding data handling practices, and a proactive approach to cybersecurity through continuous monitoring and employee training. By carefully considering these factors, laboratories can ensure that digital pathology enhances patient care while upholding the highest standards of data security and privacy.
III. The "Bottom" of the Tub: Stability and Optimization
After navigating the initial challenges of digital pathology implementation, the laboratory enters a phase of relative stability and optimized workflow. This stage marks a critical turning point where the tangible benefits of digitization become readily apparent.
Digital pathology fosters a more streamlined workflow, leading to faster turnaround times for case reviews and diagnoses. This efficiency translates to increased productivity for pathologists and laboratory staff. The availability of digital tools, such as image analysis algorithms and quantitative measurements, contributes to improved diagnostic accuracy. Digital images can be easily shared among colleagues for consultations, tumor boards, and quality assurance activities, fostering enhanced collaboration and knowledge sharing. For example, a pathologist can instantly send a case to a colleague for a second opinion, complete with annotations, AI-generated metadata (e.g., tumor grade, cell counts, percent tumor, cellularity scores), and segmented regions of interest. This seamless exchange of information facilitates efficient and informed decision-making. Quantitative data reduces subjectivity and interobserver variability, leading to more consistent and accurate diagnoses.
Digital pathology significantly reduces administrative burdens and staffing challenges in laboratories. Tasks such as slide retrieval, storage, and shipping become less time-consuming, allowing staff to focus on more critical responsibilities. This streamlined workflow and reduced administrative overhead contributes to improved morale among laboratory personnel. Furthermore, digital pathology, combined with a validated remote office, enables a hybrid work model, enhancing pathologist recruitment and retention.
Digital pathology enables real-time quality control (QC) of histological preparations. Histotechnologists can view high-resolution images of their work on large monitors, facilitating immediate identification of potential issues such as dull microtome blades, suboptimal tissue processing, or inconsistent staining. This real-time feedback loop allows for prompt adjustments and ensures high-quality slide preparation.
This phase of stability still necessitates ongoing system maintenance, periodic software updates, and continuous performance monitoring to ensure optimal system functionality and security. A dependable vendor who provides comprehensive support and maintenance services is essential for long-term success.
IV. The "Right Side" of the Tub: The Wear-Out Phase and Obsolescence
While many digital pathology systems offer stable performance and enhanced efficiency, they are not immune to the inevitable wear-out phase, characterized by an increasing failure rate and eventual obsolescence. This phase is driven by several factors, including software incompatibility with evolving operating systems and platforms. This incompatibility cascades into functionality issues, security vulnerabilities, and system failures. Additionally, scanners, like any hardware, have a finite lifespan, and vendors eventually discontinue support for older models, making it difficult to obtain replacement parts, software updates, or technical assistance.
Furthermore, the field of digital pathology is constantly advancing, with new imaging modalities, such as improved z-stacking capabilities, whole-slide fluorescence imaging, and other emerging features, rendering existing systems inadequate for optimal diagnostic techniques.
Finally, the development of new techniques and biomarkers may necessitate higher resolution scanners, and existing scanners may lack the resolution required to visualize subtle features, limiting their diagnostic utility. This wear-out phase presents unique challenges for laboratories, as upgrading or replacing components can be costly and disruptive, requiring careful planning and resource allocation.
Furthermore, migrating data to new systems can be complex and time-consuming, demanding meticulous data management strategies to ensure data integrity and avoid data loss. To mitigate these challenges, laboratories should proactively plan for system upgrades and replacements, including budgeting for future expenses, staying informed about emerging technologies, and establishing a replacement schedule for hardware components. Early engagement with preferred vendors is advisable to discuss upgrade paths and ensure quality performance from existing systems. Establishing a robust data migration strategy is also essential to ensure seamless transfer of data to new systems while maintaining data integrity and accessibility. This may involve data archiving, format conversion, and rigorous validation procedures to prevent data loss or corruption during migration.
Finally, fostering a culture of continuous learning and adaptation within the laboratory allows staff to stay on top of technological advancements and adapt to evolving needs, ensuring the long-term viability and sustainability of their improved digital workflow.
V. Mitigating the "Bathtub" Effect: Contingency Planning
To maximize the benefits of digital pathology and ensure its long-term success, a proactive approach with a robust contingency plan is essential. This plan should encompass a comprehensive risk assessment to identify potential points of failure. These vulnerabilities include hardware malfunctions, software issues, network outages, power failures, and cybersecurity breaches. Additionally, the assessment should consider potential administrative or patient-related challenges, such as delays in turnaround time (TAT).
Ensuring a continuous and stable power supply is critical for uninterrupted scanner operation. Medical-grade uninterruptible power supplies (UPS) connected to each scanner and its associated computer safeguard against data loss during power outages. This allows the system to complete ongoing scans before shutting down and facilitates secure data backup and disaster recovery procedures, ensuring business continuity.
Establishing clear alternative workflows is crucial to maintain diagnostic services during any system downtime. This may involve reverting to traditional microscopy for urgent cases or utilizing back-up scanning equipment if available. A well-defined process will minimize disruptions to patient care and ensure timely diagnoses.
Clear communication channels are vital for reporting issues, escalating problems, and keeping stakeholders informed. This includes establishing a designated point of contact for technical support and promptly notifying laboratory staff, clinicians, and, if necessary, patients about any potential delays or disruptions in service. Effective communication minimizes confusion and maintains trust among all parties.
Strong vendor support is crucial in mitigating downtime and ensuring prompt resolution of technical issues. Service level agreements (SLAs) with vendors should guarantee timely support and maintenance. These agreements should clearly define response times, escalation procedures, and service guarantees, ensuring a reliable support system for the digital pathology system.
Finally, the contingency plan for digital pathology must be periodically reviewed and updated to adapt to evolving needs, emerging technologies, and new challenges. Regularly evaluating the plan's effectiveness and incorporating lessons learned from any disruptions, whether minor incidents or major outages, will ensure its continued relevance and efficacy. This iterative process should include a comprehensive assessment of current procedures, identification of potential vulnerabilities, and implementation of necessary adjustments. Furthermore, simulating potential disruptions and observing the response of the department or laboratory can be a valuable exercise. Such simulations not only enhance preparedness but also provide insights into the strengths and weaknesses of the existing contingency plan, facilitating continuous improvement and optimization.
VI. The bathtub curve provides a valuable framework for understanding the challenges and opportunities in digital pathology implementation. By anticipating potential issues at each stage and implementing proactive mitigation strategies, labs can successfully navigate the transition and unlock this transformative technology's full potential. While careful planning, continuous improvement, and a well-defined contingency plan are crucial, proactive planning is paramount for seamless and successful integration. This approach empowers laboratories to overcome implementation hurdles and harness the power of digital pathology to drive efficiency, enhance diagnostic accuracy, and improve patient care. Digital pathology is more than just an upgrade, it is a transformation. By understanding the phases of implementation and embracing proactive strategies, you can lead your laboratory into a new era of efficiency, accuracy, and improved patient care.
Author
Scott Kilcoyne
DigitCells Cofounder & COO
For Reliability Engineering purposes, the curve is divided into three distinct phases:
- Early Failure Phase: This initial phase is characterized by a high but rapidly decreasing failure rate. Failures in this stage are typically caused by manufacturing defects, design flaws, or improper installation. Think of it like a "burn-in" period, weaker components are weeded out.
- Useful Life Phase: The middle portion of the curve shows a constant and relatively low failure rate. Failures during this phase are often unpredictable and occur randomly due to external factors or just chance. This is the period when the product is most dependable and operates as expected.
- Wear-out Phase: In the final phase, the failure rate increases again as components age and degrade. This is due to wear and tear, fatigue, and the accumulation of stress over time. The product is reaching the end of its designed lifespan.
Similar to most technological implementations, the journey towards a digital pathology lab is not without its challenges. These challenges often follow the same predictable pattern. The bathtub curve provides a valuable framework for understanding the phases of digital pathology implementation. Here's how it connects:
- Early Failures (Implementation Challenges): The initial phase represents the challenges of integrating a new technology. This could include technical difficulties, user adoption hurdles, quality control, workflow disruptions, or integration issues with existing systems. In Clinical Engineering, this is the digital pathology burn-in.
- Random Failures (Ongoing Maintenance): This is the useful stage of digital pathology. Once the system is established, you will encounter occasional issues that require troubleshooting and maintenance. These might be software bugs, hardware failures, or user errors, but the system provides the improved care and efficiencies we planned on.
- Wear-out Phase (Obsolescence): The wear-out phase represents the inevitable obsolescence of digital pathology systems, necessitating upgrades or replacements. This phase arises from several factors, including technological advancements, the evolving needs of pathology practice, and the termination of vendor support. The latter can pose significant challenges, particularly when initial budget constraints limit the acquisition of robust systems utilizing scanners from manufacturers with a proven record of enduring quality and sustained support.
II. The "Left Side" of the Tub: Early Implementation Challenges
In the beginning phases of digital pathology implementation, users will typically encounter a series of technical and workflow-related obstacles. Technical considerations primarily revolve around image quality and scanner variability. While certain scanners demonstrate superior performance in capturing specific features, such as H. pylori organisms, others may exhibit limitations when digitizing cytology specimens. Even with FDA-approved, high-end scanners, suboptimal images can occur, manifesting as blur, artifacts, or inconsistencies due to factors such as poor coverslipping, tissue folds, or debris on the slide.
Implementing a robust and user-friendly scanner calibration system is essential for achieving consistent and reliable image quality. Automated calibration enables control over color rendering, staining intensity representation, and tissue visualization. By promptly identifying and correcting performance deviations, such a system ensures the acquisition of high-quality images suitable for rigorous analysis and interpretation. This enhances the accuracy and reliability of image-based data in research and clinical settings.
While artificial intelligence (AI) solutions offer promising tools for quality control in digital pathology, their performance is not yet flawless. It is important to acknowledge that many current systems employ augmented intelligence approaches, often lacking true neural network architecture. These systems rely on predefined rules and algorithms to identify potential quality issues, which can lead to limitations in their adaptability and accuracy, especially when faced with the complexity and variability of histological preparations.
Consequently, augmented intelligence systems in digital pathology often require human oversight and intervention. Technicians may need to review and validate the quality assessments made by the system, potentially leading to rescans or image adjustments. Despite these limitations, augmented intelligence tools can still significantly benefit digital pathology workflows by automating initial quality checks and assisting technicians in identifying areas that require further attention. As AI technology continues to evolve, we can expect integrated explainability, with more robust and adaptable solutions that further enhance quality control processes in digital pathology.
To fully harness the transformative potential of AI in digital pathology, a forward-thinking approach to implementation is essential. Pathologists should proactively engage in strategic planning that encompasses current and future AI requirements, recognizing the evolving nature of AI algorithms and their expanding applications within the field. This provides a thorough evaluation of scanner compatibility with a spectrum of algorithms, ensuring the chosen system possesses the capacity for integration with both existing and emerging image tools. Moreover, the computational burden imposed by AI mandates consideration of data storage and processing infrastructure. A failure to adequately provision for these demands can bring performance bottlenecks and impede the realization of AI's full capabilities within the pathology workflow.
The integration of digital pathology with existing laboratory information systems (LIS), electronic health records (EHR), and hospital information systems (HIS) presents significant challenges. Maintaining data integrity is paramount, and rigorous validation is necessary to ensure the accurate transfer of information between these systems. Of particular concern is the potential for discrepancies between scanned microscopic areas and their corresponding macroscopic images. Such errors, which I have observed firsthand, underscore the current limitations within the field of digital pathology and highlight the critical need for high-quality manufacturing processes, stringent data integrity validation, and continuous system monitoring.
Furthermore, limitations in network bandwidth and storage capacity can impede seamless workflow. Inadequate planning for rescans and duplicate images can overwhelm local storage solutions (e.g., servers, USB backups, network-attached storage), while inefficient data management practices can lead to increased cloud storage costs. Software bugs and compatibility issues can also arise, requiring proactive troubleshooting and vendor support.
Proactively addressing potential challenges and implementing robust workflows are crucial for smooth transitions. A common hurdle, as many of us have experienced, is staff resistance to new technology. I recall a specific instance a few years ago involving a senior neuropathologist who initially favored traditional microscopy for visualizing subtle neuronal inclusions, believing digital pathology lacked the necessary detail. This presented an opportunity to emphasize the importance of comprehensive training, and with appropriate workflow adjustments, the neuropathologist quickly became a proponent of digital pathology. Such transitions often require ongoing support and patience. Fortunately, continuous advancements in scanner technology, staining techniques, and AI-powered image analysis are steadily enhancing the visualization and analysis of even the most subtle microscopic features.
Successful implementation of digital pathology extends beyond technical considerations and necessitates the establishment of standardized protocols and robust security measures to address concerns around data privacy and cybersecurity. Within healthcare, collaboration with a vendor who prioritizes patient information protection and possesses a thorough understanding of cybersecurity threats is crucial. This includes demonstrated compliance and understanding of relevant regulations like HIPAA, use of robust security measures such as encryption and access controls, transparency and accountability regarding data handling practices, and a proactive approach to cybersecurity through continuous monitoring and employee training. By carefully considering these factors, laboratories can ensure that digital pathology enhances patient care while upholding the highest standards of data security and privacy.
III. The "Bottom" of the Tub: Stability and Optimization
After navigating the initial challenges of digital pathology implementation, the laboratory enters a phase of relative stability and optimized workflow. This stage marks a critical turning point where the tangible benefits of digitization become readily apparent.
Digital pathology fosters a more streamlined workflow, leading to faster turnaround times for case reviews and diagnoses. This efficiency translates to increased productivity for pathologists and laboratory staff. The availability of digital tools, such as image analysis algorithms and quantitative measurements, contributes to improved diagnostic accuracy. Digital images can be easily shared among colleagues for consultations, tumor boards, and quality assurance activities, fostering enhanced collaboration and knowledge sharing. For example, a pathologist can instantly send a case to a colleague for a second opinion, complete with annotations, AI-generated metadata (e.g., tumor grade, cell counts, percent tumor, cellularity scores), and segmented regions of interest. This seamless exchange of information facilitates efficient and informed decision-making. Quantitative data reduces subjectivity and interobserver variability, leading to more consistent and accurate diagnoses.
Digital pathology significantly reduces administrative burdens and staffing challenges in laboratories. Tasks such as slide retrieval, storage, and shipping become less time-consuming, allowing staff to focus on more critical responsibilities. This streamlined workflow and reduced administrative overhead contributes to improved morale among laboratory personnel. Furthermore, digital pathology, combined with a validated remote office, enables a hybrid work model, enhancing pathologist recruitment and retention.
Digital pathology enables real-time quality control (QC) of histological preparations. Histotechnologists can view high-resolution images of their work on large monitors, facilitating immediate identification of potential issues such as dull microtome blades, suboptimal tissue processing, or inconsistent staining. This real-time feedback loop allows for prompt adjustments and ensures high-quality slide preparation.
This phase of stability still necessitates ongoing system maintenance, periodic software updates, and continuous performance monitoring to ensure optimal system functionality and security. A dependable vendor who provides comprehensive support and maintenance services is essential for long-term success.
IV. The "Right Side" of the Tub: The Wear-Out Phase and Obsolescence
While many digital pathology systems offer stable performance and enhanced efficiency, they are not immune to the inevitable wear-out phase, characterized by an increasing failure rate and eventual obsolescence. This phase is driven by several factors, including software incompatibility with evolving operating systems and platforms. This incompatibility cascades into functionality issues, security vulnerabilities, and system failures. Additionally, scanners, like any hardware, have a finite lifespan, and vendors eventually discontinue support for older models, making it difficult to obtain replacement parts, software updates, or technical assistance.
Furthermore, the field of digital pathology is constantly advancing, with new imaging modalities, such as improved z-stacking capabilities, whole-slide fluorescence imaging, and other emerging features, rendering existing systems inadequate for optimal diagnostic techniques.
Finally, the development of new techniques and biomarkers may necessitate higher resolution scanners, and existing scanners may lack the resolution required to visualize subtle features, limiting their diagnostic utility. This wear-out phase presents unique challenges for laboratories, as upgrading or replacing components can be costly and disruptive, requiring careful planning and resource allocation.
Furthermore, migrating data to new systems can be complex and time-consuming, demanding meticulous data management strategies to ensure data integrity and avoid data loss. To mitigate these challenges, laboratories should proactively plan for system upgrades and replacements, including budgeting for future expenses, staying informed about emerging technologies, and establishing a replacement schedule for hardware components. Early engagement with preferred vendors is advisable to discuss upgrade paths and ensure quality performance from existing systems. Establishing a robust data migration strategy is also essential to ensure seamless transfer of data to new systems while maintaining data integrity and accessibility. This may involve data archiving, format conversion, and rigorous validation procedures to prevent data loss or corruption during migration.
Finally, fostering a culture of continuous learning and adaptation within the laboratory allows staff to stay on top of technological advancements and adapt to evolving needs, ensuring the long-term viability and sustainability of their improved digital workflow.
V. Mitigating the "Bathtub" Effect: Contingency Planning
To maximize the benefits of digital pathology and ensure its long-term success, a proactive approach with a robust contingency plan is essential. This plan should encompass a comprehensive risk assessment to identify potential points of failure. These vulnerabilities include hardware malfunctions, software issues, network outages, power failures, and cybersecurity breaches. Additionally, the assessment should consider potential administrative or patient-related challenges, such as delays in turnaround time (TAT).
Ensuring a continuous and stable power supply is critical for uninterrupted scanner operation. Medical-grade uninterruptible power supplies (UPS) connected to each scanner and its associated computer safeguard against data loss during power outages. This allows the system to complete ongoing scans before shutting down and facilitates secure data backup and disaster recovery procedures, ensuring business continuity.
Establishing clear alternative workflows is crucial to maintain diagnostic services during any system downtime. This may involve reverting to traditional microscopy for urgent cases or utilizing back-up scanning equipment if available. A well-defined process will minimize disruptions to patient care and ensure timely diagnoses.
Clear communication channels are vital for reporting issues, escalating problems, and keeping stakeholders informed. This includes establishing a designated point of contact for technical support and promptly notifying laboratory staff, clinicians, and, if necessary, patients about any potential delays or disruptions in service. Effective communication minimizes confusion and maintains trust among all parties.
Strong vendor support is crucial in mitigating downtime and ensuring prompt resolution of technical issues. Service level agreements (SLAs) with vendors should guarantee timely support and maintenance. These agreements should clearly define response times, escalation procedures, and service guarantees, ensuring a reliable support system for the digital pathology system.
Finally, the contingency plan for digital pathology must be periodically reviewed and updated to adapt to evolving needs, emerging technologies, and new challenges. Regularly evaluating the plan's effectiveness and incorporating lessons learned from any disruptions, whether minor incidents or major outages, will ensure its continued relevance and efficacy. This iterative process should include a comprehensive assessment of current procedures, identification of potential vulnerabilities, and implementation of necessary adjustments. Furthermore, simulating potential disruptions and observing the response of the department or laboratory can be a valuable exercise. Such simulations not only enhance preparedness but also provide insights into the strengths and weaknesses of the existing contingency plan, facilitating continuous improvement and optimization.
VI. The bathtub curve provides a valuable framework for understanding the challenges and opportunities in digital pathology implementation. By anticipating potential issues at each stage and implementing proactive mitigation strategies, labs can successfully navigate the transition and unlock this transformative technology's full potential. While careful planning, continuous improvement, and a well-defined contingency plan are crucial, proactive planning is paramount for seamless and successful integration. This approach empowers laboratories to overcome implementation hurdles and harness the power of digital pathology to drive efficiency, enhance diagnostic accuracy, and improve patient care. Digital pathology is more than just an upgrade, it is a transformation. By understanding the phases of implementation and embracing proactive strategies, you can lead your laboratory into a new era of efficiency, accuracy, and improved patient care.
Author
Scott Kilcoyne
DigitCells Cofounder & COO
